Our Home Care Journey
Finding the Right Care for an ALS Patient
![]()
Disclaimer: This is in no way medical advice. We are not doctors and have no professional medical training. Brian has had ALS since 2011. Based on what we have learned and what works for us, we share what we know with the hope of helping increase awareness of the reality of life with a trach, ventilator and ALS.
I have started writing about this so many times. It’s a tedious topic and one that frustrates me to no end. No one should have to live like this! The emotional stress of watching Brian suffer with ALS alone is monumental. Add to that the physical demands of around the clock care giving and it’s enough to break a person. On top of it all is dealing with the healthcare system.
Our home care journey has been one long roller coaster ride and it continues still. There’s no way to calculate the time I’ve spent trying to find the best care that is also covered by insurance. I’ve created comparison charts to ensure we pick the best options for us. I have spreadsheets with hundreds of lines documenting contacts made and actions taken as they relate to Brian’s care. We lose quality time together because we are constantly fighting the system for benefits that Brian qualifies for without question.
One call leads to another and another, paperwork has to be completed, doctors orders need to be requested. The list goes on and on. Sadly, the people on the other end don’t often fully understand the situation and therefore are unable to respond adequately or with a genuine sense of urgency, and sometimes without any empathy at all.
I’ve come to the conclusion that the healthcare system (we live in the U.S.) is simply not set up to care for someone like Brian in the home, long term. Most patients prefer to be in the comfort of their own homes, surrounded by family and friends and all the things they love. Wouldn’t you? Yet finding home care has become a huge challenge.
Here in the states, if you have an acute, long term illness like ALS, I’ve got two words for you. Good luck.
That being said, there are good people and organizations out there. It’s going to be up to you to find them and it won’t always be easy. In fact, I’ve felt desperate and things have felt quite bleak at times. Persistence is key. It’s exhausting and frustrating…on top of the exhaustion and frustration of being a caregiver.
The purpose of this post is to help raise awareness about what families are having to deal with, in addition to suffering the pain of watching a loved one being taken by a brutal and merciless disease. At the same time I also hope this helps other caregivers and patient advocates feel less alone or unique in their struggles with navigating a complex and often cold and callous system. Maybe some of the terms and experiences here will help as well.
You might be asking yourself why someone would want to endure such days of pain and suffering. Wondering what’s it all for? There are plenty of good days in there too, with lots of smiles and laughter and ‘normal’ stuff. So there are good days and bad days. Just like everyone one else who is going through life, wondering what it’s all about.
We don’t know! But we’re here, we’re breathing, we wake up each day and do it all again. And we try to find joy in each day, just like everyone else.
Why? Because we want to LIVE! We just need a little more help doing it than everyone else. Brian has ALS but other than that he’s healthy. He’s vibrant. He’s funny and loves movies and music and hanging out with friends. We’re going to do everything we can to ensure he keeps doing that comfortably for as long as he can, while also not losing everything financially.
All right, so let’s get to it.
OVERVIEW
As I began working on this topic, I intended to do a quick overview of each service and talk a little bit about our experience with each one. I am going to do that here first. Then I’m going to spend some time documenting each service in detail, along with a few of the specific stories that were exceedingly frustrating at the time. There are some doozies, and some that will leave you scratching your head.
I’ll be adding links to each section as I write more about each one at a later time. For now, here is a timeline with a brief overview from diagnosis until present.
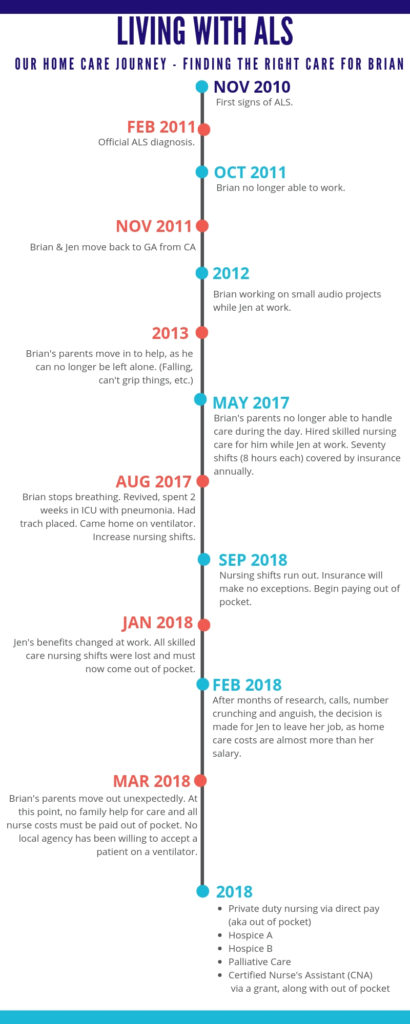
Brian was diagnosed in 2011. We managed to care for him at home without any paid home help until 2017. How we got Private duty nursing via direct pay (aka out of pocket)Certified Nurse’s Assistant (CNAthat far is another story and one we’ll share in detail another time. Here, we’re taking about paid home care. Here are the services we’ve utilized until now.
Private duty nursing via insurance
Private duty nursing via direct pay (aka out of pocket)
Certified Nurse’s Assistant (CNA) via a grant
Hospice A
Hospice B
Palliative Care
Skilled care via direct pay
It’s a lot, I know. Keep in mind we are now in year nine of Brian’s ALS, so he is in the advanced stages of the disease. He is also completely paralyzed with a feeding tube, trach and ventilator.
You might only utilize one service. You might utilize a few. It’s all just going to depend on so many things. As anyone who has ever worked for me will tell you, I have very high standards. Of myself and of others. That has led to issues with the home care companies. Brian and I have agreed together to let many of them go for one reason or another. We’ll get into more detail about that later as well.
Let’s start with a summary and general feeling about the services. We’ll take a deeper dive into each one but for now this might help to know what to even ask about.
1. Private duty nursing via insurance
May 2017 – Sep 2018
Our first experience with home care was to have a registered nurse (RN) in our home, paid for by private insurance. This benefit is called private duty nursing (PDN).
Private duty nursing is also called skilled nursing or skilled care, and it’s just what it sounds like. An RN comes to your home and cares for the patient. Most of the nurses we had through PDN would do just about anything for Brian except cut his nails. That was against their company policy, for infection/liability reasons.
A lot depends on the home care company itself but if you have PDN in your insurance plan, it’s a great benefit to utilize. Just remember that home care and skilled care are different. A lot of times home care might just mean and aide coming for an hour or so. Skilled care is more involved than that, and you should be able to leave the patient alone with an RN, meaning you can go to work or run errands. You probably won’t be able to leave the patient alone with an aide.
Honestly, and I hate to say it, but I’m not sure how many policies even have PDN as a benefit any more. (We lost this benefit from our insurance plan in 2018.)
My recommendation is to start by calling your insurance company and asking if they have this benefit, then ask for a list of their approved home care agencies. Start doing research about each one. I typically do a Google search for the company, then try and find user/patient reviews and go from there.
Once you pick one or two, you’ll call them and tell them you want to start services. They will request orders from the doctor. Then they’ll come out and do an assessment and you’ll go from there.
Note: It often feels like you should start with your doctor to get a test or service or whatever, but again, I highly recommend calling your insurance company first to ensure that the said test/service/whatever is covered or in network. If it’s not, ask the insurance company for a list of approved/in-network options.
2. Private duty nursing via direct pay (aka out of pocket)
Sept 2017 – Jan 2018
In August of 2017 Brian quit breathing. He was revived and rushed to ICU where he spent two weeks recovering from pneumonia, along with having his trach placed. At that time we were already close to running out of those 70 nursing shifts. When Brian came home we arranged for continuous care for 48 hours. That ate up a few shifts quickly.
My employer worked with me and was very flexible, allowing me to work from home one day per week, along with some shifted hours. Still, by October we were out of shifts covered by insurance. As many calls as I made and people I pleaded with, no more shifts would be covered.
In order for me to go to work, we had to have a nurse at home each day while I was gone. We paid close to $20,000 out of pocket to cover the remainder of that year. We scraped by to cover January then I took a leave of absence from work and was at home, caring for Brian. In March, I finally turned in my official resignation.
3. Certified Nurse’s Assistant (CNA) via a grant
March 2018 – May 2018
Present
It took months but I was able to utilize a grant from the GA chapter of the ALSA. I had to be the one to put in the time and effort to make it happen but they did cover three shifts for us, which allowed me to attend a wedding and a concert, and to get our van serviced.
Those three shifts were between March and May of 2018. We had a scary incident and I ended up firing our home care company because of it. We were able to get shifts covered via a grant, and very grateful for it, yet it was something we had to work for, and spend time on, arranging the care, finding the care, making the calls, etc.
Around those three shifts I was the primary caregiver 24 hours a day, 7 days a week. The stress of my job was gone and that was a huge relief, though full time caregiving can quickly start to take a toll, mostly due to sleep deprivation. But we were together and happy about that and figured we would get new home care lined up soon.
There was a big gap after firing our home care company and finding another nurse we trusted to be able to utilize this grant. We have used this again for another three shifts so far.
4. Hospice A
June 2018 – November 2018
Typically when you hear the word hospice you think about the end. Hospice is usually called in when treatment is being refused or if a doctor can tell that the body is shutting down. The service is utilized to keep the patient comfortable, the family informed and to provide a peaceful setting when leaving this place.
Though this is typically the case, I’d read many caregivers talk about how they were using hospice services for their PALS (person with ALS), and how hospice was a good fit for them.
One main benefit is that hospice services are covered by just about any insurance, including Medicare. Considering the financial strain ALS puts on families, this news can come as such relief!
Another great thing is that services are performed in the home, versus having to go out. Taking Brian out for one doctor appointment can take all day, and is stressful and exhausting for both of us.
Of course, with something that sounds so great, guess what? There’s a catch. When on hospice, most insurance plans will not cover preventive or routine care, or anything considered treatment of any kind.
It’s a long story and it took a long time and a lot of effort, but we got Brian approved on hospice in June. Whether an agency will accept a PALS or not is different depending on the company. Call and be nice. Ask questions, explain your situation, ask for a supervisor, be nice, but be firm and persistent.
Once on hospice a nurse would come check on Brian once a week. She checked his vitals, asked questions, etc. It was like a regular doctor visit, at our home. After a few visits we asked for those to be monthly.
As with all care, it depends on the people involved. Some companies will do things that others won’t. It’s about calling your insurance to get a list of approved hospice companies, then researching them, then calling to set up appointments to meet with them. That’s how it goes.
We used hospice so that we could be under a doctor’s care, with RN visits regularly. This also enabled us to have prescriptions written for Brian for his medications, or if he needed antibiotics or something like that.
That was it. Their home care included having an aide come out a few times a week for 45 minutes at a time to dress or bathe Brian.
We took them up on that for a few weeks but it just wasn’t worth it to interrupt our day for less than an hour of ‘help’. Aides are helpful but I couldn’t leave Brian alone with them so it didn’t make sense for us, but again, they can give a caregiver a break, so ask about those services if considering hospice.
Hospice can also coordinate things like physical therapy, social worker visits, chaplain visits, and things like that. Many offer a variety of additional services.
5. Hospice B
Less than 30 days
Enter Hospice B. They had been our first choice of hospice companies but would not accept Brian. The’d come out and done an assessment, got the doctor’s orders and paperwork, spent time working on our case, but after two rounds of that, we had to move on and went with Hospice A.
Hospice B had continued to call and what I like to call ‘recruit’ us. At least once a month the same man would call and “check in on us” because he and the admissions nurse both really liked us so much and really wanted to help us. So there were always kind of in the background while we had an active hospice company. They were so kind and caring.
Once we fired Hospice A (a long story) I called Hospice B and asked if we could try again. They were excited and said it felt like the chances were probably much better since we’d just had Brian on hospice. We went through the whole process yet a third time and that time they accepted Brian!
We were so happy but that honeymoon was over super quick. Honestly, they just didn’t seem equipped or ready to deal with Brian. Supplies were an issue right off the bat. They honestly just pissed us off so bad in the beginning that we let them go before a month was even up.
Ugh. I just felt so devastated after that, as I’d placed such faith in them for some reason. That was a huge blow. I’d done research on that company, made calls about them and felt good about the. I also felt like I’d make this great, genuine connection with the admissions nurse. She seemed so cool and so caring about us. Guess who I never heard from again?
When I asked Brian if he wanted to find another hospice company he said no, that his feeling from both of them had been ‘hurry up and die’.
6. Palliative Care
Present
After the two hospice experiences I was feeling really down. It just didn’t seem like there was anything set up in the system for our needs. I am the primary caregiver and have committed to being that for Brian yet I need to take a break from time to time. The home care journey continued.
There are labor laws in place that require breaks after certain periods of work but I’d been on duty 24 hours a day 7 days a week for almost a year, with maybe 60 hours of total relief in that time. OSHA doesn’t care about that. On top of that, Brian needs attention all through the night as well. It’s very rare that I get more than two hours of sleep at one time, and haven’t for over a year now.
Medicare covers home care but the manual specifically states that it will not cover a nurse shift so that a caregiver spouse can go to work. Isn’t that crazy?! It states a whole lot of things. It’s very complex and wordy.
If you’ve got some time, grab a cup of coffee and curl up with that baby. It’s oh so riveting. Never mind that your loved one needs attention right now, you should use your time sifting through hundreds of pages of bullshit reasons and excuses and tiny little loopholes in the plan that lead to claims and phone calls and services being denied. But I digress.
Here’s a link to the home care chapter of the Medicare policy manual. You can read and decide for yourself. Mind you, these pages of information are in addition to the 100+ page manuals that are mailed out.
( https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c07.pdf )
Anyway, after hospice I asked around and kept hearing about “palliative care” and that it was kind of a new thing that was being used instead of hospice. I contacted one of our nurses from ALS clinic and asked if they had any leads on that. They said it was something they were hearing about too and they did have a recommendation for a company they’d been working with.
Since our clinic was already familiar with that palliative care company I went ahead and called them to get the ball rolling. When starting services with any company the first thing they want after insurance info is an order from a doctor. An order is basically another way of saying prescription. The doctor needs to verify that the patient is truly in need for home care so that it can be filed with insurance.
That part was easy since the clinic and the palliative company were already familiar with one another. In just a couple of days we had an appointment for the admissions person to come out and get the initial paperwork signed.
So whatever, we were admitted and the ball was rolling on palliative care. We agreed that a monthly visit from a nurse would be fine. She came and made her initial visit. She is super sweet and caring while she is here. She is able to assess any concerns, call in prescriptions and can help us react to any issues that come up. That’s about it for her role.
In addition to a regular nurse check up visit, palliative care also offers the services of aides to come out and help with caregiving tasks. We went ahead and turned those services down. It was the same thing, where they can come out for an hour at a time at most. That’s just not the help we need and it’s just kind of annoying for both of us, to be honest.
It might sound ungrateful, but Brian wants to do what he wants with his time. Interacting with strangers or acquaintances for a brief time, where they perform caregiving tasks at a mediocre level just doesn’t help either one of us. Our goal with seeking home care was, and had been, getting temporary relief for me so that I could run errands and do things away from the house.
The tasks that aides help with are personal like dressing and bathing. It’s tough to let a stranger in and feel any kind of comfort. It’s nice to have some time to establish comfort and some trust being caregiver and patient. A rotating door of different aides just doesn’t work for Brian.
Still, they can be a huge help if they are a good fit and if it works for your situation. I strongly suggest that you try all services and see what feels right. You can always discontinue something if you don’t like it, and restart if you change your mind. Try it, then decide.
As of this initial post writing we’ve been with this company for about four months. I’d give them a 7 out of 10. There was a small issue with admissions and a few hiccups as we got set up with them.
We had an issue with Brian’s formula the very first time I ordered it and we almost ran out of his food. Yes we can feed him real food but they had no sense of urgency on his nutrition and I had to keep following up.
The second nurse visit was messed up due to scheduling/communication issues with them and the third visit was a complete disaster. A good story I will share in detail soon.
Our palliative company doesn’t offer private duty nursing and their aides don’t want be left with a ventilator patient. I don’t want to leave him with them anyway. Maybe other companies have the staff. I bet if I tried hard enough I could work with a company to help get them educated and trained. I’ve added that to my to-do list.
So yeah, they are fine, whatever. Palliative is serving the needs we have of getting prescriptions filled and getting regular checkups without having to take Brian out. It is definitely possible to go out and about with a trach and ventilator but Brian basically hates it so we don’t. I’ll write about that another time too.
While palliative was/is serving those needs mentioned above, we still had to find a way to be able to give me a break so we continued looking for a nurse (skilled care) that could be left with Brian while I stepped away for a bit.
7. Skilled Care via Direct Pay
Present
Time and time again it comes back to home care. At this point, for us, that’s what we really need help with the most. I am fine to care for Brian the majority of the time but no one could be expected to handle this level of caregiving all the time, always. It just can’t work long-term. It’s not the healthiest option for either of us. We’ve been looking for someone who is not only trained but has some experience with the ventilator. It’s something most people can do with training but it does require constant attention and a sense of urgency.
I called every agency on the Medicare approved list and none of them were staffed to take a vented patient. I talked to several people, asking if we could help train the staff or see if we could give something a try. Some people really seemed to want to help but there are liability and other issues to consider. Easier to just say no. I will continue to reach out and see if we can help them make some progress.
After I checked all the agencies off the list, I just sat there staring at that list. It felt like the end of the road. I’d read, I’d called, I’d researched…I could not find home care that was covered by insurance that would enable me to leave the house without Brian. Not long term, anyway.
The issue is then twofold. I need a break but I’m also not working so our income is extremely limited. Skilled care can run from $20-80 per hour or more. It all depends. Most nurses want a full shift of at least eight hours, so to round it out, a day shift is $200 or more. That’s a utility bill and then some. That’s a medical bill or supplies. And that’s just one shift on one day.
We don’t want to be a drain on the system. We’re not trying to have the system pay for heaps of nursing so I can go out and have a bunch of fun. We just need some help from time to time so that I can run errands, see a movie or heck, go for a walk in our neighborhood.
It’s not just leaving the house. I am Brian’s caregiver all the time. We endure things we will probably never talk about to you. You don’t want to know. It is heavy on a relationship to be put in those positions. I do it all out of love but you know those moments aren’t sparking a lot of romantic feelings for either of us.
When a nurse is here I can sit next to Brian and hold his hand and just be with him. If no one else is here I have to get up and suction him while we are watching TV or listening to a record. Having a nurse here means we can just relax together. Still, as usual, it’s a catch-22. We can just chill together and I don’t have to get up, but we’re not alone. Ugh. ALS, you asshole!!
Not just ALS but the healthcare system. It’s hard to understand how we’ve gotten to this point. But now, it’s a matter of navigating through it, which is incredibly frustrating and stressful.
So that’s our home care journey so far. Hope that helps in some way, if nothing more than to add perspective to the plight of an ALS battle. And we press on.
We Are Not Alone
Our story is uniquely ours, yet shares a lot of common themes with other families battling ALS. Each state is different and each agency is different as well, each with different staff and experience levels. This does give you a taste of what it’s like navigating the healthcare system in the States.
A friend once said to me, “You are one illness away from losing everything.” I hadn’t ever thought of it in quite that way but she is right. Scary, isn’t it? It really is true.
Think about it. If you got sick, like really sick and ended up like Brian, paralyzed and on a ventilator, who would care for you? Another person would need to be within earshot of you every minute of every day. If you had to pay someone twenty dollars an hour to do that, would you have that saved up?
Financial strain is one part of dealing with a long term illness. Emotional strain is another. Physical strain comes along with being a caregiver. All of these things and we haven’t done better for ourselves. Instead, we spend time battling red tape and bureaucratic BS instead of helping ourselves in our time of need. We (collective) add a parallel journey to the long and heavy one we’re already on, marred by complex language and fear of liability versus humans stepping up and helping each other.
Good luck to those having to deal with these issues. Here’s to your strength and patience. Share your experiences or tips as well. We’d love to hear them!



