THE SYSTEM IS BROKEN
Before I get into my musings on this topic I’d like to first share a story that can hopefully provide a bit of context about things in general. An example that’s fresh in my mind, as it just happened recently.
A few weeks ago, Brian’s body decided that it didn’t like the formula he’d been taking for many months. For some reason, he just stopped tolerating it. We gave it a few (very long) days, just to see if it was a stomach virus or something like that. We switched to only real food for a bit. Each time we introduced the formula back into the mix, it was clear that his body was just over it.
So. You assess the situation. No fever, vitals normal and stable, root cause, then solution identified. We needed to try a different formula. Brian’s formula, a.k.a. food is a prescription. Insurance (Medicare) requires a prescription for formula.
In the event that the formula needs to change, Medicare requires a note from the doctor. In this case, they wanted a face to face visit with the doctor before they would approve it. Just to get different food!
Taking Brian to Emory literally takes a day. Planning, prep, loading, travel, unload. It’s hard to describe how hard that is on him.
Brian’s had ALS since 2011. It is documented over and over. No one in their right mind could ever assess him and say anything different. He’s been in the system, coded as having ALS for almost ten years. There is no doubt about his condition. The issue is that the system does not understand that.
When I told other caregivers, “Brian hasn’t been tolerating his formula and his stomach is upset,” they empathized immediately because they knew what that meant,. Hell for both of us. Hours of dealing with the impacts of an upset stomach and a completely paralyzed body. I’ll leave it at that and pray you never have to do it yourself.
And yet, telling Medicare that he stopped tolerating his formula requires us to jump through hoops just to try something different.
It took over a month from the first contact to our doctor to when we received the new formula on our doorstep. A month. (As frustrating as that all was, keep reading, as this all ties into the silver lining at the end!)
I blend foods for Brian but having formula saves time and effort and is a huge part of our care routines. It also has high calories. Blending your own food can be tough, to get it the right consistency for the tube, as well as having enough calories before Brian doesn’t want anymore because he’s full.
The point is that in a perfect world, the system would know Brian has ALS, a call could be made and bam, we have what we need. Because we need it! It’s hard to describe the frustration that comes with this kind of bullshit red tape all the time. Oh, and sprinkle in some real jerks who lost their empathy a long time ago, and then it’s just a whole new level of frustration.
Wait, we’re paying for this?! Yes, we pay for Medicare. It’s not free. It’s just like any other insurance. We pay premiums and co-pays and deductibles. Medicare is not free and is different than Medicaid. Either way, they’re both part of the same system and seriously…
The system is broken.
You hear those words and they may or may not resonate with you. Based on our experience navigating the US healthcare system with ALS in the last ten years, here’s what I think.
If you’re wealthy or a veteran, you’ve got a head start. If not, and certainly if you have no insurance, the fight is going to be even harder. (Not that vets have it made.)
A disease like ALS takes advocates fighting hard for the patient all the time, just for what is right and fair, based on the system guidelines themselves.
I’m an Army brat. My father served over 20 years, and so did my grandfather, both serving in wars, as well as my brother in the Navy. Those men, along with our families, have made sacrifices. My childhood is steeped in the system. I grew up with the government as our guide.
The military dictated where we lived, and many other aspects of our lives. It was all around me as a child. Office buildings with the same metal desks and the same standard-issue black pens. Hierarchies and salutes, processes and procedures, pomp, and circumstance.
There’s a feeling of pride that comes along with all of that as well. When I think about it, I’m sure all of that gave me some sort of deep-seated belief in that system. That if you worked hard and paid into it, that it would yield the return of that work and contribution, even when in the private sector, as you’d be contributing by paying taxes, social security, etc.
Not so much.
If Brian had been a vet, things might be a little different. But he was a dream chaser and a damn good one. He quit college in our last semester and went to school to be an audio engineer instead. That was his passion and he went for it! He then landed himself an internship at Triclops, a major label studio in Atlanta, and that’s where we planted our roots. We’ve lived a happy life together.
Though neither of us served in the military or worked in a federal position, Brian and I have still worked hard and paid into the system. I worked full time from the time I graduated from college in 1996 until I was forced to walk away from Honda in 2018. And do you know why that happened? Pay attention here…
Because a few years ago the government decided that it would be a good idea to fine a company for having benefits that were “too good”. Hefty fines. Millions. It’s called a Cadillac Tax, though as of this writing it has still not gone into effect. For real, Google it!
Let’s go through that again, shall we?
The government was telling some corporations that their health insurance plans were too good and that if they didn’t change those benefits to be not so good, then the company would be fined. So a company takes care of its people and the government steps in to say don’t do that or you’ll pay. What kind of crazy shit is that?!
As companies do, my employer sought to protect its bottom line and our insurance benefits changed. That change left us with a policy that suddenly did not include skilled home care (also called private duty nursing). That was someone to care for Brian while I was at work. That benefit alone was equal to $23,520 out of our pocket annually.
Imagine that your favorite person in the world is sick and paralyzed, relying completely on you and others for care.
Imagine you are trying to keep the job that has the insurance for you both. How many nurse shifts would you need to be covered in order to stay working?
I thought some charts might help visualize some of this. Plus, I love making this kind of stuff!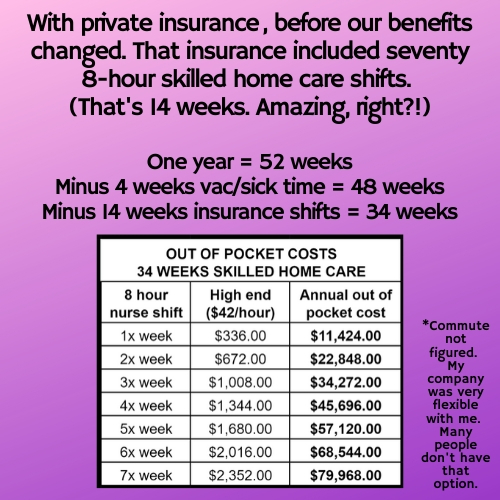

 The difference in the hourly rate in the charts comes down to where we were/are getting help. The agency that could handle Brian AND had a nurse that could stay with Brian while I left the house was pricy. Their hourly rate billed to insurance was $42 per hour, and it was the same rate for us.
The difference in the hourly rate in the charts comes down to where we were/are getting help. The agency that could handle Brian AND had a nurse that could stay with Brian while I left the house was pricy. Their hourly rate billed to insurance was $42 per hour, and it was the same rate for us.
You can see here that even with good private insurance, the cost to keep working would have been astronomical. As much as I earned, it wasn’t enough. I could give all my income to a nurse, paid for out of pocket, or I could quit, lose my own insurance and we could live off our life savings. One other option was to put Brian in a facility, and I will do everything I possibly can to keep that from ever happening. So I walked away from my career and here we are.
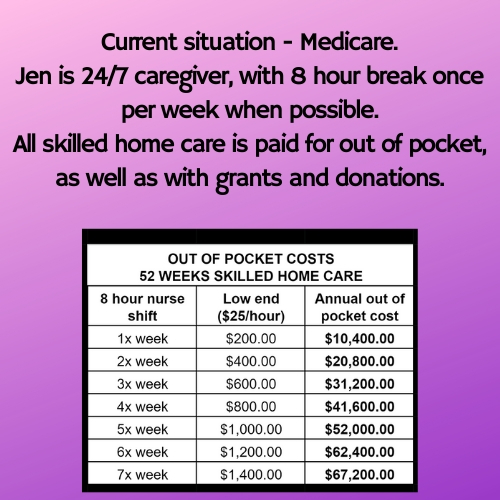
Once I left my job and we only had Medicare, we couldn’t use our original agency for a variety of reasons, so we found help ourselves. (Not that we could afford $42 per hour anyway!)
Time and time again it has felt like such a slap in the face when dealing with the system and the people in it. Red tape and greed end up causing so much suffering to those who rely on the system. For those who had faith that it could even be a crutch or supplement it just feels like such a farce.
We don’t need massive amounts of money from the system at this point. We’re not, nor have we ever, asked for the system to just straight-up support us. We built savings over time and never expected to ask for a full, free ride. At this point I’d just like an 8-hour break from time to time or heck, maybe even a couple of days off, like normal jobs provide but that’s not easily possible either.
By now, I’ve literally spent weeks on the phone, completing paperwork, filing claims, and the like, just to claim benefits for which Brian qualifies, and is absolutely entitled to. For anyone with a terminal diagnosis, all you want to do is make the best of the time you have left. You want to spend quality time doing the things you love with the people you love. Having to navigate such a cold and complex system takes so much valuable time away from simply being with the ones you love, providing support and comfort.
When I think about it, my mind has such a hard time understanding how we are all within such a horrible system, yet we humans are the ones that created this hot mess.
Overall, the healthcare system is just a false sense of security and broken AF. I’ve cried so many tears and screamed into the air after getting off the phone with yet another person who doesn’t give a flip. The stories we could tell you would make your jaw drop.
One day I’ll tell you in detail the stories of Marla and Robin, two of our home care nurses that behaved in ways that I can’t for the life of me understand. We almost kicked Marla out of our house, and Robin ghosted us after a week of service, never to be heard from again. W…T…F?!?!
We’ve had Brian on with several agencies and none of them could truly support the needs of an ALS patient on a ventilator. Most agencies are so scared of the liability issues associated with a ventilator that they won’t even take that kind of patient on, and the ones we begged to onboard with ended up being let go for one reason or another because they just were not at all the right fit for Brian and his ALS.
While the ventilator seems like such a scary thing, it’s also not rocket science. The tube in Brian’s throat gets mucus in it and it requires another person to use a machine to suck it out. I have ZERO medical experience and a three-hour crash course on caring for someone on a ventilator, and I’ve become a pro at it. (Mind you, it was very thorough and amazing training. Thank you, Rob!)
Brian says I’m better than anyone that’s done it for him. That sounds dirty, tee hee…😉🤣
Over time I’ve learned how to suction Brian’s trach just like any other nurse would. Practice and experience are the keys when it comes to suctioning a trach. Most people could learn and get a feel for it over some time. Push air into Brian’s lungs so that he takes a bigger breath than his body can do for him, then force that air and mucus back out by forcing a cough with the machine. Just like any other task in the world, you learn how to do it, practice, and get better.
Yes, it’s nerve-racking knowing that you’re responsible for another being, but so is taking care of kids, the elderly, and other dependents. Even pets. Something else relies on you. Another life is your responsibility. You learn how to provide the care that’s required, then it becomes second nature. Same with suctioning the trach and caring for an ALS patient.
It’s hard to understand how the system so easily presents patients with the option for a trach and to live longer on a ventilator, yet there is no support system in place for that. Caregivers are completely left out of the equation. Someone that’s paralyzed has to have at least one other person to help care for them 24/7. For a diagnosis like ALS, the primary caregiver really needs to be added to the big picture. They aren’t sick but become as trapped by the disease as the patient, albeit in extremely different ways.
And yet, with that knowledge being widely documented, there are no provisions within the system for someone with ALS. Patients with the disease are forced to navigate a system that has not caught up with the demands of the disease. Preventative appointments and regular processes just don’t work for this disease. Like making a patient like Brian jump through hoops to get different food. I invite anyone in authority within the Medicare system to please come to spend 48 hours with us and see the brutal reality of this disease. Surely changes would be made in haste.
What’s always been weird to me is that ALS is one of two things that will get you shortlisted for Social Security Disability. The regular waiting period is shorter for those with ALS and those with renal failure. And yet, after that, simple needs or change requests require such an effort on the part of the patient and of the doctors and their staff. So many things just don’t make any sense, and again…spending time on administrative items takes valuable time away with our loved ones who are dying in front of our very eyes.
I could go on for days but that’s enough for now. I need to be better about sharing stories in real-time. You’d just be shocked at what the system has put us through. Sadly, so many others could write the exact same words. It breaks my heart for all of us.
Silver lining. While the system is terribly broken, I believe the coronavirus could be a turning point toward improvement.
For the first time in a very long time, I have hope! Hope that things can be greatly improved. AND…we’re already seeing some effects of this.
But guess what?! Remember how we needed that “face to face” appointment in order to get new formula for Brian? Before Covid-19 we would have had to have taken Brian to an office somewhere. It’s hard to describe the effort it takes for both of us to travel, so we’ll just say it takes all we’ve got, physically and mentally.
Because of the virus we were able to do an appointment via Zoom and it. was. awesome! In just a couple of minutes we logged on and got to speak with Brian’s doctor face to face, discussing recent issues, as well as how Brian was doing overall. It was comfortable, relaxed and saved us an entire day. It’s hard to describe the relief we felt being able to get the appointment in without having to load Brian up and take him out. If he’s going to make the effort to go out he wants it to be fun for him.
Just like that, after years of frustration about the system, I can see the possibility of change, which can benefit not only patients but the entire system. Imagine the resources freed up when commutes are not involved for every little thing. Telecommuting and tele-doc appointments can save time and money for everyone all around, not just in the healthcare community but in so many aspects of business. Hope, hope, HOPE!
#als #alsawareness #alsawarenessmonth #tendaysofals



